Would you like to work for a great company? Apply here
Click Here for COVID-19 Updates and visitation policies at our facility
Barnegat Rehabilitation and Nursing Center Outbreak Response Plan is based upon national standards and developed in consultation with our infection control committee.
Our protocol for isolating and cohorting infected and at risk patients in the event of an outbreak of a contagious disease until the cessation of the outbreak these are described in the following Policy and Procedures and/or Protocols : Coronavirus Disease (COVID-19) Identification and Management of Ill Residents, Infection Prevention and Control Measures, Isolation – Categories of Transmission-Based Precautions and Cohort Plan.
Methods to communicate information on mitigating actions implemented by the facility to prevent or reduce the risk of transmission, including if normal operations of the facility will be altered. Notifications shall not include personally identifiable information; these are described in the following Policy and Procedures and/or protocols:
Infectious Disease Threat Communications Plan
Methods to provide cumulative updates for residents, their representatives, and families of those residing in the facilities at least once weekly in particular during a curtailed visitation period:
Infectious Disease Threat Communications Plan
Written Standards, policies and procedures that provide for virtual communication (e.g. phone video-communication, Facetime, etc.) with residents, families, and resident representatives, in the event of visitation restrictions due to an outbreak of infectious disease or in the event of an emergency which are described in the following proprietary policies, procedures, and protocols:
Facilitating Video Visits, Cleaning and Disinfection of Mobile Technology Devices protocol, Coronavirus Disease (COVID-19) Visitors
A documented strategy for securing more staff in the event of a new outbreak of COVID-19 or any other infectious disease or emergency among staff which is described in the following Policy and Procedures, and/or protocols:
Emergency Staffing Plan, Coronavirus Disease (COVID-19) – Surge Capacity Staffing
Information on the availability of laboratory testing, protocols for assessing whether facility visitors are ill, protocols to require ill staff to not present at the facility for work duties, and processes for implementing evidence-based outbreak response measures which are described in the following proprietary policies, procedures, and protocols: Lab and Diagnostic Test Results – Clinical Protocol, Test Results, COVID-19 Testing Protocol, Coronavirus Disease (COVID-19) Education and Training, Coronavirus Disease (COVID-19) Identification and Management of Ill Residents, Coronavirus Disease (COVID-19) Reporting Facility Data to the Centers for Disease Control and Prevention, Infection Prevention and Control Program, Outbreak of Communicable Diseases, Surveillance for Infections, Coronavirus Disease (COVID-19) Visitors, Limited Visitation During the COVID-19 Pandemic
Policies to conduct routine monitoring of residents and staff to quickly identify signs of a communicable disease that could develop into an outbreak which are described in the following
proprietary policies and procedures: Coronavirus Disease (COVID-19) Infection Prevention and Control Measures, Coronavirus Disease (COVID-19) Identification and Management of Ill Residents, Coronavirus Disease (COVID-19) Prevention and Control, Infectious Disease Threat Surveillance and Detection, Infectious Disease Threat, Infection Control Measures During, Employee Infection and Vaccination Status, Surveillance for Infection
Policies for reporting outbreaks to public health officials in accordance with applicable laws and regulations which are described in the following proprietary policies and procedures: Coronavirus Disease (COVID-19) Reporting Facility Data to the Centers for Disease Control and Prevention, Coronavirus Disease (COVID-19) Identification and Management of Ill Residents, Coronavirus Disease (COVID-19) Prevention and Control, Reporting Communicable Diseases, Infection Prevention and Control Committee, Infection Prevention and Control Program, Infectious Disease Threat Surveillance and Detection, Outbreak of Communicable Diseases.
If you would like additional information about our response to COVID-19 or other infectious disease threats please contact us at (609) 698-1400
Outbreak Procedure
Policy Statement:
Outbreaks of communicable diseases within the facility will be promptly identified and responded appropriately to decrease the risk of transmission to residents and staff, which has the potential to pose a significant public health threat and danger of infection to the residents, resident representatives, and staff of the facility.
As required by the State Department of Health, the facility's outbreak response plan is built to fit to the facility's needs. It is based upon national and state standards and developed in consultation with the facility's infection control committee. The facility's plan includes but shall not be limited to:
1. A protocol for isolating and cohorting infected and at-risk residents in the event of an outbreak of a contagious disease until the cessation of the outbreak.
2. Policies for the notification of residents, residents' families, guardians, visitors, and staff in the event of an outbreak of a contagious disease at a facility.
3. Information on the availability of laboratory testing, protocols for assessing whether facility visitors are ill, protocols to require ill staff to not present at the facility for work duties, and processes for implementing evidence-based outbreak response measures.
4. Policies to conduct routine monitoring of residents and staff to quickly identify signs of a communicable disease that could develop into an outbreak; and
5. Policies for reporting outbreaks to public health officials in accordance with applicable laws and regulations.
Outbreak- is defined as any unusual occurrence of disease or any disease above background or endemic levels.
Endemic Level- means the usual level of given disease in a geographic area.
Pandemic - A sudden infectious disease outbreak that becomes very widespread and affects a whole region, a continent, or the world due to a susceptible population. By definition, a true pandemic causes a high degree of mortality.
Emerging Infectious disease -- Infectious diseases whose incidence in humans has increased in the past two decades or threatens to increase in the near future have been defined as "emerging." These diseases, which respect no national boundaries, include:
• New infections resulting from changes or evolution of existing organisms
• Known infections spreading to new geographic areas or populations
• Previously unrecognized infections appearing in areas undergoing ecologic transformation
• Old infections reemerging as a result of antimicrobial resistance in known agents or breakdowns in public health measures
Isolation – Separation of an individual or group who is reasonably suspected to be infected with a communicable disease from those who are not infected to prevent the spread of the disease.
Cohorting- means the practice of grouping patients who are or are not colonized or infected with the same organism to confine their care to one area and prevent contact with other patients.
Quarantine – Separation of an individual or group reasonably suspected to have been exposed to a communicable disease but who is not yet ill (displaying signs and symptoms) from those who have not been exposed to prevent the spread of the disease.
Outbreak Phases:
A. Pre-outbreak phase:
The facility's Infection Control Preventionist (ICP) will be vigilant and stay informed about infectious diseases worldwide and update the Outbreak Plan as needed as new communicable diseases develop.
• The Outbreak Plan will be maintained in the Emergency Disaster Plan and Infection Prevention and Control Manual.
• The facility's Infection Control Committee (ICC) will serve as the authority for outbreak preparedness and response. The ICC comprises of the Medical Director, Infection Control Preventionist, Administrator, Director of Nursing, Director of Environmental Services, and Human Resources
• The facility will maintain an adequate emergency stockpile of personal protective equipment (PPE), including moisture-barrier gowns, face shields, surgical masks, assorted sizes of disposable N95 respirators, and gloves; essential cleaning and disinfection supplies so that staff, residents, and visitors can adhere to recommended infection prevention and control practices.
• Addressing Engineering controls in coordination with the facility administrator for any appropriate physical plant alterations such as use of private rooms for high-risk residents, plastic barriers, sanitation stations, and special areas for contaminated wastes as recommended by local, State, and federal public health authorities.
B. Outbreak Heightened Alert Phase:
• This phase begins when a confirmed case of communicable disease is detected in the community.
• The Infection Control Preventionist will keep administrative leadership briefed as needed on potential risks of new infections in their geographic location through the changes to existing organisms and/or immigration, tourism, or other circumstances.
• Assess the facility stock pile of PPE, necessary supplies and equipment and review staffing contingency plans.
• Assess the availability of vaccines, antiviral medications, and other essential medications from the pharmacy, DHS, as well as state stockpile.
• Identify crucial gaps in infrastructure, resources and policies that may interfere with an effective response. Action will be taken to resolve.
• Staff will be educated on the exposure risks, symptoms, and prevention of the infectious disease, with special emphasis on reviewing the basic infection prevention and control, use of PPE, isolation, and other infection prevention such as hand washing.
• If infectious disease is spreading through an airborne route, then the facility will activate its respiratory protection plan to ensure that employees who may be required to care for a resident with suspected or known case are not put at undue risk of exposure.
• Provide residents and families with education about the disease and the facility's response strategy at a level appropriate to their interests and need for information.
• Brief vendors/contractors on the facility's policies and procedures related to minimizing exposure risks to residents
• Establish a command center using the Infection Control Preventionist as coordinator. The Infection Control Preventionist will maintain frequent contact with the Administrator, the Medical Director, and Director of Nursing.
• The administrator and or the Director of Nursing will hold a Staff Meeting to alleviate fear and answer staff concerns.
• Post signs regarding hand sanitation and respiratory etiquette and/or other prevention strategies relevant to the route of infection at the entry of the facility along with the instruction that anyone who is sick must not enter the building.
• The Infection Control preventionist will meet with the Clinical team and other essential personnel to keep them informed and prepare them for any changes in their daily activities that may be anticipated. Re-education such as hand washing, donning and doffing of PPE, respiratory protection plan and etc., will be conducted.
• Alert the Food Service Department to assess the need to stockpile food and water.
• Review environmental cleaning procedures and frequency such as terminal disinfection, high touch areas, equipment, common areas and other.
• Staff that are exhibiting signs and symptoms of communicable disease, will be sent home and will follow self-isolation and return to work protocol.
• Inform each department to review staffing contingency plans for any anticipated absenteeism and illness.
• The Infection Control Preventionist will initiate Line Listing as a mechanism to track specific infectious disease and symptoms in residents and employee illness related absenteeism increases that might indicate early cases of outbreak
• Identify and Screen residents, staffs and visitors, based on the outbreak identified.
• Isolate and or cohort residents with signs and symptoms of infectious disease following the facility's isolation/cohort plans and in accordance to NJDOH and CDC guidance.
• Screening and or Diagnostic Testing will be done as warranted to identify specific infectious disease.
• The Social Service Department will reach out to local Funeral establishments to establish contact and procedures in coordination with the Infection Control Preventionist.
Screening Protocol:
A. Staff Self Screening -Staff will be educated on the facility's plan to control exposure to the residents. This plan will be developed with the guidance of public health authorities and may include:
• Reporting any suspected exposure to the Infectious Disease while off duty to their supervisor and Infection Control Preventionist.
• Precautionary removal of employees who report an actual or suspected exposure to the infectious disease.
• Self-screening for symptoms prior to reporting to work.
• Prohibiting staff from reporting to work if they are sick until cleared to do so by
appropriate medical authorities and in compliance with appropriate labor laws.
• Will communicate with the Infection Preventionist nurse and or the Director of Nursing for clearance to return to work.
• Facility shall screen and log HCP and everyone entering the facility for symptoms of the infectious disease.
Screening will include:
• Temperature checks, including subjective and/or objective fever equal to or greater than 100.4 degrees Fahrenheit or as further restricted by the facility.
• Completion of questionnaire about symptoms and potential exposure and travel history in the affected geographic areas listed by the State DOH of the date of the screening entry and close confirmed contact to a confirmed infected person e.g. COVID-19 infection.
B. Residents and Visitors – Identify and Screen residents and visitors, based on the outbreak identified.
Residents:
• Facility will conduct active screening of all residents: • Nursing Staff will monitor residents daily for symptoms of infectious disease including monitoring of vital signs.
• Specific symptoms of infectious diseases will be identified and all residents will be monitored for these symptoms, as well as history of travel in affected geographic areas listed by the State DOH of the date of the visit within 14 days of onset, (or if otherwise specified by CDC).
• Resident will be monitored for signs and symptoms related to the infectious disease for those having confirmed close contact with someone that was infected.
Visitors:
• Facility will conduct active screening of all visitors EXCEPT EMS personnel.
o These services can continue with a policy for services to be rendered in a safe manner to include but are not limited to infection control and precautions, physical distancing, hand hygiene, cleaning between clients for the barber/hairstylist, and the use of well-fitting source control.
o The facility will advise everyone who enters the building to monitor for signs and symptoms of COVID 19 for at least 14 days after exiting the facility and if symptoms to self isolate at home and call us immediately to alert the ICP/Administrator immediately as to when they were in the building last and whom they visited with and where they visited. The facility will screen the individual/s who are a reported contacts and implement necessary actions based on the findings.
o The facility MUST receive written, informed consent from visitors that they are aware of the possible dangers of exposure to COVID 19 for both the resident and the visitor, and that they will follow the visitation rules set by the facility.
- A copy of the consent form must be provided to visitors confirming that they are aware of the risk of exposure to COVID 19 during the visit. than 100.4 degrees Fahrenheit or as further restricted by the facility.
o Visitors MUST strictly comply with the policies of visitation.
o Visitors MUST notify the facility upon receipt of a positive COVID 19 test result or exhibiting symptoms of COVID 19 that develop within 14 days of the visit.
o The facility will have a designated area for visitors to log in and be screened.
· Screening Protocol to consist of a completion of a questionnaire about symptoms and potential exposure which shall include at a minimum:
o Whether in the last 14 days, the visitor has had an identified exposure to someone with a confirmed diagnosis of COVID 19, someone under investigation for COVID 19, or someone with respiratory symptoms.
o Whether the visitor has been diagnosed with COVID 19 and has not yet met criteria for the discontinuation of isolation per guidance issued by DOH and CDC.
o Whether the visitor is experiencing;
- Fever
- Chills
- Cough
- Shortness of Breath or difficulty breathing
- Sore Throat
- Fatigue
- Muscle or body aches
- Headache
- New loss of taste or smell
- Congestion or runny nose
- Nausea or Vomiting
- Diarrhea
· Visits NOT allowed
o Have current COVID 19 infection
o Have symptoms of COVID 19
o Have had close contact with someone with SARS CoV-2 infection in the prior 14 days or have otherwise met criteria for quarantine or
o If viral testing (i.e. antigen or PCR) is used and tests positive
- You cannot mandate testing of visitors but it may be offered upon entrance prior to visitation
C. Source Control:
• Universal Masking for all staff and visitors will be required when entering the facility as directed by the ICP.
• All visitors will maintain social distancing, six feet apart, while at the facility unless the resident is fully vaccinated and choses close contact.
• Visitors are encouraged to perform hand hygiene prior to visiting and will observe respiratory etiquette protocols.
D. Outbreak Phase:
This phase begins when there is a confirmed case of communicable disease in the facility following the outbreak definition in accordance to NJDOH guidance.
• The Infection Control Preventionist (ICP) will direct the facility's planning and response efforts and is responsible for surveillance and is in constant contact with the local and State Department of Health and notification of cases in accordance to mandated NJDOH, CDC reporting for communicable diseases.
a. During the infectious disease outbreak, mechanisms for monitoring employee absenteeism for increases that might indicate early cases of an outbreak will be utilized.
b. Line listings will be utilized as mechanisms for tracking facility admissions and discharges of suspected or laboratory-confirmed cases of the specific infectious disease outbreak in residents to support local public health personnel in monitoring the progress and impact of the outbreak
c. Assess bed capacity and staffing needs, and detect a resurgence in cases that might follow the first wave of cases
d. Update information on the types of data that should be reported to the state agency and/or local health departments (e.g., admission; discharges/deaths; resident characteristics such as age, underlying disease, and secondary complications;
e. Monitor illnesses in healthcare personnel and plans for how this data will be collected during an outbreak
f. Establishes criteria for distinguishing the type of outbreak from other respiratory diseases.
• The Infection Control Committee (ICC) will work with the ICP and assist with decision-making during an outbreak.
• Adhere to Standard and Transmission-based Precautions including use of a facemask, gown, gloves, and eye protection for confirmed and suspected case(s).
• Provide all assigned staff additional training and supervision in the mode of transmission of this ID, and the use of the appropriate PPE.
• Assign dedicated staff to enter the room of the isolated person as feasible. Ideally, only specially trained staff and prepared (i.e. vaccinated, medically cleared, and fit tested for respiratory protection) will enter the isolation room.
• Implement the isolation protocol in the facility (isolation rooms, cohorting) as described in the facility's infection prevention and control plan and/or recommended by local, state, or federal public health authorities.
• Activate quarantine interventions for residents and staff with suspected exposure as directed by local and State public health authorities and in keeping with guidance from the CDC.
• Suspend or limit visits on the affected unit/area.
• Administer available vaccines and antivirals according to a priority group
COHORTING: The facility will cohort residents as follows and as directed by the State Department of Health and the CDC:
• Cohort 1 –Positive for Infectious disease outbreak. (COVID 19)
• This cohort consists of both symptomatic and asymptomatic patients/residents who test positive for COVID-19, regardless of vaccination status, including any new or re-admitted patients/residents known to be positive who have not met the criteria for discontinuation of transmission-based Precautions. If feasible, care for COVID-19 positive patients/residents on a separate closed unit. Patients/residents who test positive for COVID-19 are known to shed virus, regardless of symptoms; therefore, all positive patients/residents would be placed in this positive cohort.
• Cohort 2 – Unvaccinated, Exposed:
• This cohort consists of symptomatic and asymptomatic patients/residents who test negative for COVID-19 with an identified exposure (i.e., close contact) to someone who was positive, regardless of vaccination status. This includes new or re-admitted patients/residents who have tested negative and have been identified as a close contact in the past 14 days. Exposed individuals should be quarantined for 14 days from last exposure, regardless of negative test results or vaccination status. All symptomatic patients/residents in this cohort should be evaluated for causes of their symptoms. Patients/residents who test negative for COVID-19 could be incubating and later test positive. To the best of our ability, the building will separate symptomatic and asymptomatic patients/residents, ideally having symptomatic housed in private rooms. Even though symptomatic COVID-19 negative patients/residents might not be a threat to transmit COVID-19, they still may have another illness, such as influenza. Asymptomatic patients/residents should be closely monitored for symptom development. Unvaccinated patients/residents who are identified as close contacts should be quarantined for 14 days and have a series of two viral tests. In these situations, testing is recommended immediately (but not earlier than 2 days after the exposure) and, if negative, again 5–7 days after the exposure. If testing is negative, the patient/resident should be tested again 5-7 days after exposure. If testing remains negative, patients/residents should complete the remainder of their 14-day quarantine period. Testing at the end of this period could be considered to increase the certainty that the person is not infected.
· Fully vaccinated patients/residents identified as close contacts* should continue to follow the Centers for Disease Control and Prevention (CDC) infection prevention and control measures, including wearing well-fitting source control, getting tested as described above, and monitoring for symptoms for 14 days after exposure.
• Cohort 3 – Negative, Not Exposed:
• This cohort consists of patients/residents who test negative for COVID-19 with no COVID-19 like symptoms and are thought to have no known exposures. This cohort includes all individuals who have clinically recovered from SARS-CoV-2 within 90 days of symptom onset or positive test, and all fully vaccinated individuals who have not been in close contact with a suspected or known COVID-19 case. The index of suspicion for an exposure should be low, as COVID-19 has been seen to rapidly spread throughout the post-acute care setting. In situations of widespread COVID-19 transmission in a facility, all negative persons in a facility would be considered exposed. Cohort 3 should only be created when the facility is relatively certain that patients/residents have been properly isolated from all COVID-19 positive and incubating patients/residents and HCP. Given facility-wide transmission levels, Cohort 3 may or may not be applicable.
• Cohort 4 – New or Re-admissions observation:
• Unvaccinated, not up to date with all recommended COVID-19 doses, new or readmission observation (quarantine): These individuals consist of all unvaccinated and and not up to date with COVID-19 vaccine; new patients/residents from the community or other healthcare facilities and unvaccinated and not up to date with COVID-19 vaccine, re-admitted patients/residents who left the facility for ≥24 hours. This cohort serves as an observation area where persons remain for 10 days to monitor for symptoms that may be clinically compatible with COVID-19. Testing at the end of this period could be considered to increase the certainty that the person is not infected. In most circumstances, quarantine is not recommended for unvaccinated or not up to date with all recommended COVID-19 Dose, patients/residents who leave the facility for <24 hours and do not have close contact with a suspected or known COVID-19 positive person.
• EXCEPTIONS TO CONSIDER:
o Individuals who remain asymptomatic have met the criteria for discontinuation of transmission-based precautions for SARS-CoV-2 infection, and it has been <3 months after the date of symptom onset or positive viral test (for asymptomatic) of prior infection generally require no further restrictions based on their history of COVID-19.
o Consideration needs to be given to determine whether there is concern that there may have been a false positive viral test, whether the patient/resident is immunocompromised, and whether there is evidence of exposure to a novel SARS-CoV-2 variant.
o If a patient/resident experiences new symptoms consistent with COVID-19 and an evaluation fails to identify a diagnosis other than SARS-CoV-2 infection (e.g., influenza), then repeat viral diagnostic testing and isolation may be warranted even if they have clinically recovered within three months.
o Healthcare facilities should continue to follow the infection prevention and control recommendations for unvaccinated individuals when caring for fully vaccinated individuals with moderate to severe immunocompromise due to a medical condition or receiving immunosuppressive medications or treatments. This includes using transmission-based precautions for those who have had close contact with someone with SARS-CoV-2 infection.
Outbreak recommendations
In the event of widespread identified cases, the focus should be placed on Cohorts 1 and 2.
In situations where COVID-19 positive persons are located on multiple units/wings, the facility should follow the below recommendations:
Implement universal transmission-based Precautions using COVID-19 recommended PPE (i.e., NIOSHapproved N95 or higher level respirator [or well-fitting facemask if unavailable], eye protection, gloves, and isolation gown) for the care of all patients/residents, regardless of the presence of symptoms or COVID-19 status.
• Refer to CDC Optimizing PPE Supplies at https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe/strategy/index.html
o These strategies offer a continuum of options for use when PPE supplies are stressed, running low, or exhausted.
o Optimization strategies are meant to be considered and implemented sequentially (i.e., conventional > contingency > crisis). o Healthcare facilities should promptly resume conventional or standard practice as PPE availability returns to normal.
• Consider repurposing unused space such as therapy gyms, activity and dining rooms during this time to cohort patients/residents. Refer to the NJDOH COVID-19 Temporary Operational Waivers and Guidelines at https://www.nj.gov/health/legal/covid19/.
• If there are multiple cases on the wing/unit and when movement would otherwise introduce COVID19 to another occupied wing/unit, do not relocate them. Ensure appropriate use of engineering controls such as curtains to reduce or eliminate exposures from infected individuals. Rapid isolation is key. Once there are multiple cases or exposures on a wing/unit, transition the wing/unit to the appropriate cohort and focus efforts on rapid implementation of control measures for unaffected wings/units (i.e., containment efforts).
• When spacing permits, COVID-19 positive individuals should be relocated to the dedicated COVID-19 positive area (Cohort 1). Otherwise, limit the movement of all patients/residents and HCP in general.
• Ensure appropriate use of engineering controls, such as curtains between patients/residents to reduce or eliminate exposures from infected individuals. This is especially important when semi-private rooms must be used. Allocate private rooms to maintain separation between patients/residents based on test results and clinical presentation. For example: o COVID-19 positive persons may share a semi-private room to keep them grouped together.
Patients/residents who are colonized with or infected with multidrug-resistant organisms (MDROs), including Clostridium difficile, should not be placed in a semi-private room or group area when possible, unless their potential roommate(s) is/are colonized or infected with the same organism(s). o Private rooms may be allocated to isolate COVID-19 positive persons or quarantine close contacts, based on availability.
• Prioritize maintaining dedicated HCP to a wing/unit with a heightened focus on infection prevention and control audits (e.g., hand hygiene and PPE use) and providing feedback to HCP on performance
- Documentation of outbreak-
a. Date and time of the first sign or symptom, when testing was conducted, when results were obtained, and the actions taken based on the results
b. Document the time and date of a new COVID 19 case in the facility, document the date the case was identified, the date that other residents and staff are tested, the dates that staff and residents who tested negative are retested, and the results of all tests.
Laboratory Testing:
• Facility has a contract agreement in-place with a licensed laboratory company to perform laboratory testing.
· If a 48 hour turn around time cannot be met for results, the facility will document all efforts to obtain the quicker turn around results with the identified laboratory and contact the localand state department of health
• The facility has access to BinaxNow rapid tests as well.
• Diagnostic testing to identify specific infectious disease and testing for infectious diseases such as COVID-19 for residents will be conducted in consultation with the local and State departments, the resident primary physician/ Medical Director and in accordance with the State Department of Health, CDC and other applicable regulatory testing requirements.
• The resident, resident representatives, and the physician will be informed when performing a diagnostic or surveillance testing.
• Routine testing and other appropriate diagnostic and surveillance testing for all staff including vendors will be conducted in accordance with the State Department of Health, CDC and other applicable regulatory testing requirements.
- Documentation of testing-
- Staff
- Name
- Date of testing
- Result of each test
- Resident
- Order to do the testing
- Documentation in the EMR
- Testing was offered
- Completed
- Results of the testing
• Staff or residents that have tested positive will not require further testing for 90 days from the date of their positive test
• Staff who test positive will return to work as per the CDC guidelines and when appropriate to their previous position
• Refusal of Testing-
o Resident Refusal
Shall treat the individual as a PUI
Make a notation in the resident's chart
Notify any authorized family members or legal representatives of this decision.
Continue to check temperature on the resident at least twice per day
Onset of temperature or other symptoms consistent with COVID-19 require immediate cohorting in accordance with the Plan.
At any time, the resident may rescind their decision not to be tested.
o Employee Refusal
Employee will be removed from the schedule as this is a requirement of employment.
When prioritizing individuals to be tested, prioritizing individuals with signs and symptoms of COVID-19 first, then perform testing triggered by an outbreak investigation (as specified below).
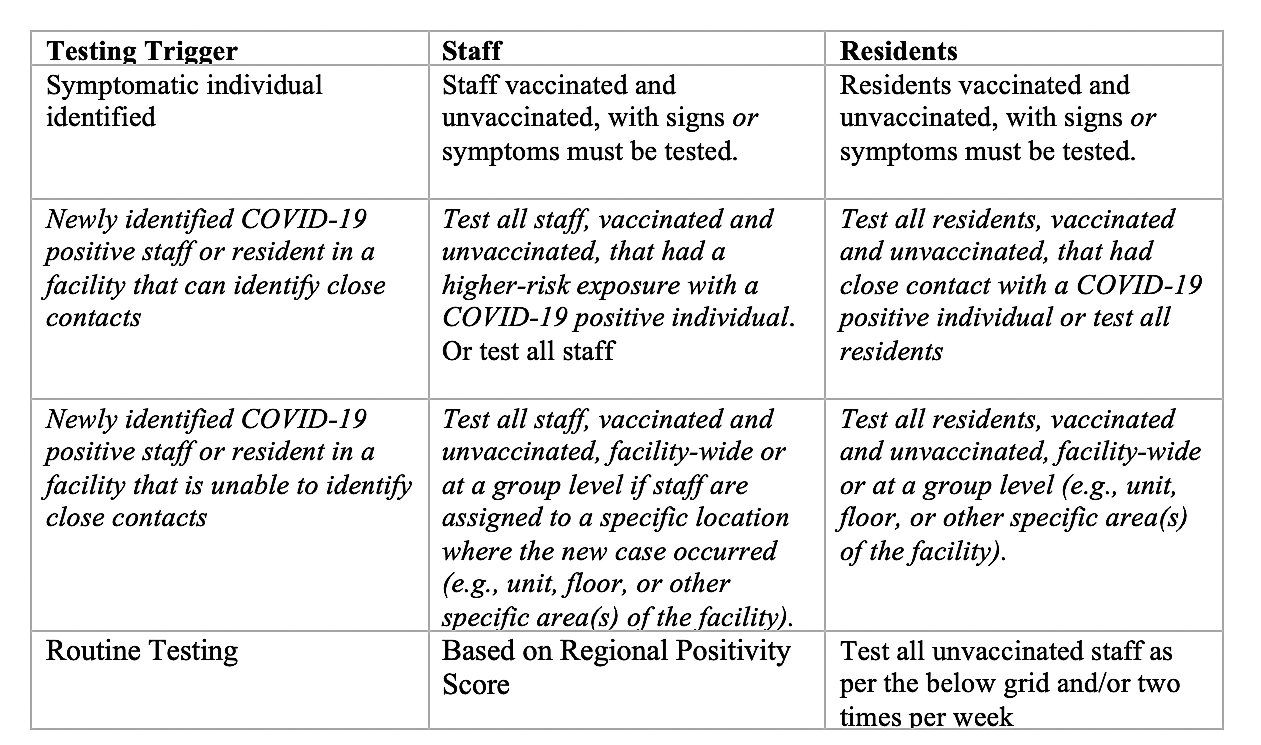
TESTING PROCEDURES AND FREQUENCY
- Facilities may use any viral testing (e.g. PCR or antigen) and collection method (e.g. swab or saliva) approved by the United States Food and Drug Administration (FDA)
- During moderate and high community transmission scores, facility may request but not require, visitors to be tested on their own prior to coming to the facility (e.g. within 2-3 days) with proof of negative results and date of test: the visitor can provide proof of a negative FDA approved or authorized point-of-care test collected and performed in the past 24 hours or PCR test collected and resulted no more than 3 days prior to the visit
- Facilities that have POC testing available are encouraged to use it as part of their visitor screening process, in particular during high/very high Community Transmission scores in the region. Visitors who test positive are not permitted to enter the building
- Routine testing should be based on the extent of the virus in the community, therefore facilities should use the regional positivity rate report in the COVID-19 Activity Level Index (CALI) weekly Report: https://www.nj.gov/health/cd/statistics/covid/
- Use the prior week to determine testing frequency
- Regional CALI Level/ Regional % Positivity rate in past week Minimum Testing
- Cali scores Community transmission Testing
- Low <3% Once a week
- Medium <3-10% Once a week
- High/Very High >10% Twice a week
- Further retesting will be completed in accordance with CDC guidance, as amended and supplemented. The facility will consider establishing a routine interval of retesting.
- Staff that are fully vaccinated do not need to be tested unless symptomatic and/or the building is in outbreak testing of all staff
Communication Methods:
The facility will prominently display the facility's website and or social media platforms to include communication to resident representatives and the public and provide a phone number or method of communications for urgent calls or complaints.
• Social worker or facility designated staff will be assigned as a primary contact to families for inbound calls and will conduct a regular call at least weekly to keep families up to date; this may include virtual visitation, conference calls, e-mails, phone calls, and etc. Create and maintain an email list serve.
• Facility will provide alternative methods of communication to include phone, video-communication, Facetime and etc., with residents and families, and resident representatives. The facility designated person will serve as a "visual coordinator" to arrange, coordinate time schedules with residents and families
• The facility will provide a cumulative update for residents and resident representatives, and families at least once weekly through letters or email listserv communications during a curtailed visitation period. The updates will include information about any infectious disease outbreaks as required by NJDOH, information on mitigating actions implemented by the facility to prevent or reduce the risk of transmission, to include if facility normal operations will be altered.
• Administrator or facility designated staff will host conference calls or virtual calls at a minimum once weekly. Time will be set when families can call or log on to a conference line to share the status of activities or update happenings in the facility. Family members will be encouraged to make suggestions or ask questions during the calls.
• The administrator and or facility designated staff will update website, at a minimum on a weekly basis, to share the status of the facility and information that helps families to know what is happening in the facility's environment, such as food menus, schedule activities, and etc.
• Administrator or facility designated staff will notify each resident and resident representative by 5 pm the next calendar day following the occurrence of a single confirmed COVID case or three or more residents or staff with new-onset respiratory signs and symptoms within 72 hours of each other, and follow state, federal guidelines regarding notification of other infectious diseases.
Outbreak Reporting:
• In the event of an outbreak, the facility will immediately report/notify and consult with the Local/State Public Health Department for specific directions.
• The Infection Control Preventionist and/or the facility administrator is the designated staff to report to the local and State Department of Health and notify cases in accordance to NJDOH, CDC according to applicable laws and regulations in reporting for communicable diseases.
• The administrator and or the Infection Control Preventionist will notify the Medical Director, resident, resident representatives, and staff for any occurrence of an outbreak and mitigating actions implemented by the facility through resident in person notification by the Social worker or designee during resident council meetings, signage, emails, memos, facility website, family/resident representatives weekly calls, and staff in-services, phone calls or staff group text messaging.
• The facility will report to National Healthcare Safety Network (NHSN) two times per week during an outbreak
o Counts of residents and facility personnel with-
Suspected cases
Confirmed cases
o Counts of facility personnel whose death is
Suspected to have been caused by the infectious disease
Confirmed by a laboratory test to have been caused by the infectious disease
o Total number of residents
o Current resident census
o Staffing shortages
o Quantity and number of days the current inventory will last
Personal protective equipment
Hand hygiene supplies
Cleaning supplies
Sanitation supplies
o Any other metrics that the Commissioner deems appropriate
o Flu season
Employees who received the flu vaccine
Employees who declined flu vaccine due to medical reasons with an authorized medical exemption
Employees who declined the flu vaccine NOT due to medical reasons
Staffing Strategies:
• Assign a facility representative for conducting daily assessment of staffing status and needs during a staffing shortage
• All employees in the facility will be notified of the decision to utilize emergency staffing strategies.
• Cancel all non-emergency procedures or outpatient consults
• Review staffing protocols and consistent assignment
• List essential staff/positions
• List non-essential staff/positions
• Assigning non-direct care to support staff and or administrative staff.
• Utilizing nursing school graduates to assist with patient care.
• Utilizing nursing students for non-direct care and or
• Contract with local Staffing Agencies to secure staff
• Overtime and other incentivized strategies
• Hire non license support staff to assist nursing for non-direct care. Be aware of state-specific emergency waivers or changes to licensure requirements or renewals for select categories of HCP.
• Infection Preventionist and Human Resource will continue to follow through with employees who are out sick or furloughed related to COVID-19 screening to return to work if cleared following CDC and DOH guidelines.
• On call rotation for management staff
• Cancellation of vacation or day off
• Recruiting retired health care workers
• 12- hour shifting for Nurses and CNA's
• Develop task force teams, Nurses, CNA's management staff to work during staffing crisis
• Determine business interruption and virtual work options.
• The hiring of Medical Technicians (MRT) and Certified Home Health Aides (HHA) to function as a role of CNA's following NJDOH temporary nurse staffing waiver related to COVID-19 State of Emergency plan.
• Attempt to address social factors that might prevent HCP from reporting to work, such as transportation or housing if HCP live with vulnerable individuals.
Post Outbreak Phase:
• The Infection Control Preventionist will coordinate with the local and or State Department of Health the cessation of an outbreak.
• The Infection Control Committee will convene and assess the response of the outbreak and make adjustments to the plan, as appropriate (with recommendations from NJDOH).
• The facility will return to Pre- Outbreak phase.
Visitation:
Outdoor Visitation: While taking a person-centered approach and adhering to the core principles of COVID-19 infection prevention, outdoor visitation is preferred when the resident and/or visitor are not fully vaccinated3 against COVID-19. Outdoor visits generally pose a lower risk of transmission due to increased space and airflow.
a. For outdoor visits, facilities should create accessible and safe outdoor spaces for visitation.
b. Weather considerations (e.g., inclement weather, excessively hot or cold temperatures, poor air quality) or an individual resident’s health status (e.g., medical condition(s), COVID-19 status, quarantine status) may hinder outdoor visits.
c. When conducting outdoor visitation, all appropriate infection control and prevention practices should be followed.
Indoor Visitation: Facilities must allow indoor visitation at all times and for all residents as permitted under the regulations.
a. While previously acceptable during the PHE, this facility will no longer limit the frequency and length of visits for residents, the number of visitors, or require advance scheduling of visits.
b. Although there is no limit on the number of visitors that a resident can have at one time, visits should be conducted in a manner that adheres to the core principles of COVID-19 infection prevention and does not increase risk to other residents.
c. This facility will ensure that physical distancing can still be maintained during peak times of visitation (e.g., lunch time, after business hours, etc.).
d. This facility will avoid large gatherings (e.g., parties, events) where large numbers of visitors are in the same space at the same time and physical distancing cannot be maintained.
e. During indoor visitation, this facility will limit visitor movement in the facility.
a. For example, visitors will be strongly encouraged to not walk around different halls of the facility.
b. The visitor should go directly to the resident’s room or designated visitation area..
f. If a resident’s roommate is unvaccinated or immunocompromised (regardless of vaccination status), visits should not be conducted in the resident’s room, if possible.
a. For situations where there is a roommate and the health status of the resident prevents leaving the room, this facility will attempt to enable in-room visitation while adhering to the core principles of infection prevention.
g. If this facilities county COVID-19 community level of transmission is substantial to high, all residents and visitors, regardless of vaccination status, should wear face coverings or masks and physically distance, at all times.
a. In areas of low to moderate transmission, the safest practice is for residents and visitors to wear face coverings or masks and physically distance, particularly if either of them is at increased risk for severe disease or are unvaccinated.
h. If the resident and all their visitor(s) are fully vaccinated and the resident is not moderately or severely immunocompromised, they may choose not to wear face coverings or masks and to have physical contact.
i. Visitors should wear face coverings or masks when around other residents or healthcare personnel, regardless of vaccination status.
j. While not recommended, residents who are on transmission-based precautions (TBP) or quarantine can still receive visitors.
a. In these cases, visits should occur in the resident’s room and the resident should wear a well-fitting facemask (if tolerated).
b. Before visiting residents, who are on TBP or quarantine, visitors should be made aware of the potential risk of visiting and precautions necessary in order to visit the resident.
c. Visitors should adhere to the core principles of infection prevention.
d. Facilities may offer well-fitting facemasks or other appropriate PPE, if available; however, facilities are not required to provide PPE for visitors.
k. NOTE: CMS and CDC continue to recommend facilities, residents, and families adhere to the core principles of COVID-19 infection. This continues to be the safest way to prevent the spread of COVID-19, particularly if either party has not been fully vaccinated. However, we acknowledge the toll that separation and isolation has taken. We also acknowledge that there is no substitute for physical contact, such as the warm embrace between a resident and their loved one.
a. Therefore, if the resident is fully vaccinated, they can choose to have close contact (including touch) with their visitor in accordance with the CDC’s “Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) Pandemic.”
b. Unvaccinated residents may also choose to have physical touch based on their preferences and needs, such as with support persons for individuals with disabilities and visitors participating in certain religious practices, including in end-of-life situations. In these situations, unvaccinated residents (or their representative) and their visitors should be advised of the risks of physical contact prior to the visit.
l. Visitors should also physically distance from other residents and staff in the facility.
Indoor Visitation during an Outbreak Investigation An outbreak investigation is initiated when a new nursing home onset of COVID-19 occurs (i.e., a new COVID-19 case among residents or staff). When a new case of COVID-19 among residents or staff is identified, a facility should immediately begin outbreak testing in accordance with CMS QSO 20-38-NH REVISED and CDC guidelines. While it is safer for visitors not to enter the facility during an outbreak investigation, visitors must still be allowed in the facility.
a. Visitors should be made aware of the potential risk of visiting during an outbreak investigation and adhere to the core principles of infection prevention.
b. If residents or their representative would like to have a visit during an outbreak investigation, they should wear face coverings or masks during visits, regardless of vaccination status, and visits should ideally occur in the resident’s room.
Visitor Testing and Vaccination While not required, we encourage facilities in counties with substantial or high levels of community transmission to offer testing to visitors, if feasible.
a. If facilities do not offer testing, they should encourage visitors to be tested on their own before coming to the facility (e.g., within 2–3 days).
b. CMS strongly encourages all visitors to become vaccinated and facilities should educate and also encourage visitors to become vaccinated. Visitor testing and vaccination can help prevent the spread of COVID-19 and facilities may ask about a visitors’ vaccination status, however, visitors are not required to be tested or vaccinated (or show proof of such) as a condition of visitation.
c. If the visitor declines to disclose their vaccination status, the visitor should wear a face covering or mask at all times.
d. This also applies to representatives of the Office of the State Long-Term Care Ombudsman and protection and advocacy systems, as described below.
Compassionate Care Visits Compassionate care visits are allowed at all times. Previously during the PHE, there were some scenarios where residents should only have compassionate care visits. However, visitation is now allowed at all times for all residents.
a. There are few scenarios when visitation should be limited only to compassionate care visits.
b. In the event a scenario arises that would limit visitation for a resident (e.g., a resident is severely immunocompromised and the number of visitors the resident is exposed to needs to be kept to a minimum), compassionate care visits would still be allowed at all times.
c. This facility will not restrict visitation without a reasonable clinical or safety cause, consistent with 42 CFR § 483.10(f)(4)(v). In previous nursing home visitation guidance during the PHE, CMS outlined some scenarios related to COVID-19 that would constitute a clinical or safety reason for limited visitation. However, there are no longer scenarios related to COVID-19 where visitation should be limited, except for certain situations when the visit is limited to being conducted in the resident’s room or the rare event that visitation is limited to compassionate care. Therefore, a nursing home must facilitate in-person visitation consistent with the applicable CMS regulations, which can be done by applying the guidance stated above..
d. If a visitor, resident, or their representative is aware of the risks associated with visitation, and the visit occurs in a manner that does not place other residents at risk (e.g., in the resident’s room), the resident must be allowed to receive visitors as he/she chooses.
